Introduction
The evolution of technology in healthcare has led to the emergence of autonomous surgical systems, revolutionary tools that enhance surgical outcomes and improve patient safety. However, with technological advancements come significant regulatory challenges that must be navigated to ensure the safety and efficacy of these systems. This article delves into the regulatory pathways for autonomous surgical systems, examining existing frameworks, challenges, and future directions.
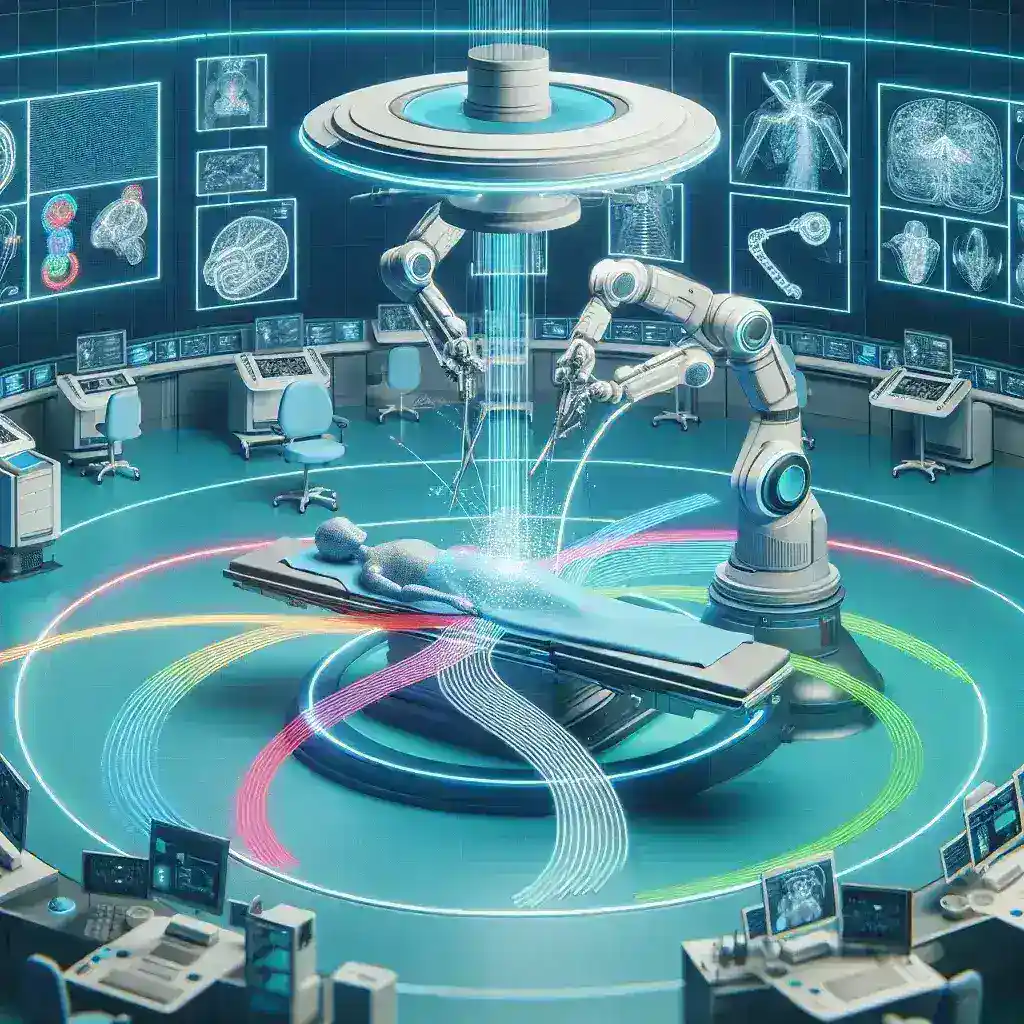
Understanding Autonomous Surgical Systems
Autonomous surgical systems refer to medical devices capable of performing surgical procedures with minimal human intervention. These systems leverage advanced technologies like artificial intelligence (AI), robotics, and machine learning to enhance surgical precision and reduce human error. A notable example is the use of robotic-assisted surgery systems that can assist surgeons during complex procedures.
Historical Context
The journey towards autonomous surgical systems began in the late 20th century with the introduction of robotic surgery. The pioneering da Vinci Surgical System, approved by the FDA in 2000, marked a significant milestone in minimally invasive surgery. Since then, numerous surgical robots have entered the market, paving the way for increasingly autonomous systems.
Current Regulatory Frameworks
1. FDA Regulations in the United States
The U.S. Food and Drug Administration (FDA) plays a crucial role in regulating medical devices, including autonomous surgical systems. The FDA classifies these devices into three categories based on the level of risk:
- Class I: Low-risk devices with minimal regulatory control, such as basic surgical instruments.
- Class II: Moderate-risk devices requiring premarket notification (510(k)) to demonstrate safety and effectiveness, including many robotic surgical systems.
- Class III: High-risk devices necessitating premarket approval (PMA) to ensure safety and effectiveness through extensive clinical trials.
For autonomous surgical systems, the classification often depends on their level of autonomy and the risks associated with their use. As technology progresses, the FDA is adapting its regulatory frameworks to address these innovations.
2. International Regulatory Bodies
Outside the United States, various international regulatory bodies oversee the approval and monitoring of medical devices. For instance, in Europe, the European Medicines Agency (EMA) and the Medical Device Regulation (MDR) dictate the standards for medical devices, ensuring they meet stringent safety and efficacy requirements before market entry. Similar frameworks are observed in other regions, like the Therapeutic Goods Administration (TGA) in Australia and the Health Canada in Canada.
Challenges in Regulatory Pathways
1. Rapid Technological Advancements
The fast-paced evolution of autonomous surgical systems presents a significant challenge to regulatory bodies. Traditional regulatory frameworks often struggle to keep up with the speed of innovation, leading to potential gaps in safety and efficacy assessments.
2. Data Privacy and Security
As autonomous surgical systems increasingly rely on data for AI and machine learning, concerns regarding data privacy and security arise. Ensuring robust cybersecurity measures to protect sensitive patient information becomes paramount, necessitating additional scrutiny during the regulatory process.
3. Standardization of Testing Protocols
The variability in testing protocols across different regulatory bodies can create inconsistencies in device approval. Lack of standardized guidelines for evaluating the performance and safety of autonomous surgical systems can hinder their global market access.
Future Directions
1. Adaptive Regulatory Frameworks
To address the dynamic nature of technology, regulatory bodies are moving towards adaptive regulatory frameworks that allow for more flexible and iterative approaches to approval. This model emphasizes continuous monitoring and real-world data collection post-implementation to ensure ongoing safety and efficacy.
2. Collaboration Between Stakeholders
Collaboration among manufacturers, regulatory agencies, and healthcare providers is vital to shaping the future of autonomous surgical systems. Engaging in dialogue can help align regulatory expectations with technological advancements, fostering innovation without compromising patient safety.
3. Emphasis on Cybersecurity
As technology continues to evolve, the focus on cybersecurity within regulatory frameworks will intensify. Ensuring that autonomous surgical systems are resilient against cyber threats will be critical for maintaining trust and safety in surgical environments.
Conclusion
The regulatory landscape for autonomous surgical systems is complex and continually evolving. By understanding the current frameworks and addressing the challenges inherent in this technology, stakeholders can work towards a future where autonomous surgical systems can be effectively integrated into clinical practice. As we move forward, a concerted effort is needed to adapt regulatory pathways to foster innovation while ensuring the highest standards of patient safety.
Call to Action
For healthcare professionals, policymakers, and industry leaders, engaging in the regulatory process is crucial. By advocating for clear and adaptive regulations, we can help shape the future of autonomous surgical systems, ensuring they benefit patients worldwide.